Redefining Baseline: The First Step to Staying Left of Bang
Sep 11, 2025Redefining Baseline: The First Step to Staying Left of Bang
Situational awareness isn’t about waiting for something big to happen—the Bang.
It’s about noticing the small shifts.
The off-pattern behaviors.
The moments that don’t line up with what we’ve come to expect.
But here’s the catch:
In order to recognize patterns and deviations and truly stay Left of the Bang, we first have to understand baseline.
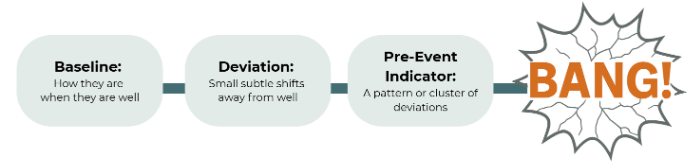
This is the Left of Bang sequence. It starts with baseline—how a resident is when they’re well. From there, we notice deviations (small shifts away from well). When deviations cluster together, they form pre-event indicators. If those indicators are missed or dismissed, they eventually explode into the Bang—a crisis, complaint, or event we could have seen coming.
The Problem with “Normal”
“Baseline” gets tossed around in clinical conversations all the time. But ask most frontline staff what it means, and you’ll hear something like:
“It’s how the resident normally is.”
Here’s the problem with that definition:
- New admissions aren’t at baseline. Most residents arrive sick, unstable, and complicated. Their first impression is not their well self. It can take days—or weeks—to uncover their real baseline.
- “Normal” hides unmet needs. Residents with dementia, trauma, or chronic conditions may express themselves in ways that don’t look “normal.” Wandering, repeating the same question, or withdrawing from others might actually be part of their baseline. But when staff rely on assumptions—or inherit biases through the grapevine—decline or distress gets written off as “just how they are.”
- “Normal” blinds you to risk. If staff define baseline as whatever they see most often—even if it’s illness—you lose the ability to notice pre-event indicators.
Redefining Baseline
Baseline isn’t “normal.”
Baseline is a resident’s personal version of well—the stable pattern that belongs to them, quirks and all.
Let’s break that down.
- Well
Baselines should be grounded in wellness, not illness.
Defining baseline when someone is unwell is like setting your watch to the wrong time—every decision you make after that is already off. You’ll miss the subtle shifts that signal risk because your starting point was wrong.
Example: A resident admitted with pneumonia may be lethargic, confused, and barely eating. If that snapshot gets stamped as their “baseline,” then weeks later when they decline again, no one catches it—because it looks the same as day one.
- Personal Version
Each person has their own “well.”
- For one resident with dementia, wearing multiple layers of clothes might be their baseline—it’s stable, familiar, and part of who they are.
- For another, showing up in three sweaters could be a glaring deviation—an early indicator that something has changed.
Baseline isn’t about the behavior itself. It’s about whether the behavior is consistent for that individual. Baseline is shaped by each resident’s history, illnesses, trauma, personality, and life journey. People don’t fit into cookie cutters, and neither do their baselines.
A Real-Life Example: The “Challenging” Resident
Here’s what this looks like in practice.
At a recent training, I asked staff to describe the baseline of a “challenging” resident they all knew. She was the reason I was doing the training.
They had been “taught” baseline informally—through the grapevine or by whoever trained them—about what to expect from her. And because they defined baseline as “how the resident normally is,” their answers were all over the place:
- “She’s mean.”
- “She’s unpredictable.”
- “She changes depending on her caregiver.”
- “She changes depending on the day.”
- “She can actually be nice and pleasant.”
They weren’t careless. They were doing their best with the definition they’d been given. But the result was the same: everyone in the room had a different version of “normal.”
Then we redefined baseline together—as her personal version of well. Suddenly the conversation shifted. Staff could describe a clearer, more consistent version of her best self, quirks and all.
I pushed them further: “How would you know if she got a UTI?”
That stopped them. Beyond the obvious physical symptoms, they admitted they might not recognize a change in her behavior—because their definition of her baseline was muddled with illness, unpredictability, or bias. If baseline is unpredictable, then every change gets lost in the noise. Their blind spot meant they could easily miss the very pre-event indicators that matter most.
Where Harm Grows
Baseline isn’t “how they normally are.” That’s not clarity—it’s a blind spot. And blind spots are where harm grows.
When leaders redefine baseline as each resident’s personal version of well, they give their teams the ability to see deviations for what they really are—early warnings, not background noise.
This is the foundation of situational awareness in nursing homes.
Get baseline wrong, and you’ll always be right of Bang.
Get it right, and you give your team the chance to act before the crisis hits.
⚡ Part 2 will dig deeper into how leaders can teach this definition, interrupt blind spots, and connect it directly to Left of Bang thinking.
And if you’re still tempted to say, “That’s just the way she is”? Read my last blog. It’ll ruin that phrase for you forever: That’s Just the Way She Is.
Feeling the shift too? Whether you're navigating change or redefining your purpose, you're not alone. Let’s build something better—together.
👉 Explore my trainings | 💬 Share your story | 📩 Connect with me today
Stay connected with news and updates!
Join our mailing list to receive the latest news and updates from our team.
Don't worry, your information will not be shared.
We hate SPAM. We will never sell your information, for any reason.

